Does Lithium Make You Blackout From Alcohol Easy
TABLE OF CONTENTS
What's Covered in this Article

Imagine what the music industry would be today if Jimi Hendrix, Whitney Houston, Jim Morrison, Amy Winehouse, and Janis Joplin had lived out the rest of their careers. All of these artists have one thing in common; they died by mixing alcohol with other drugs.
"My greatest fear is probably dying with no one knowing of any contribution I'd ever made to creative music."
-Amy Winehouse
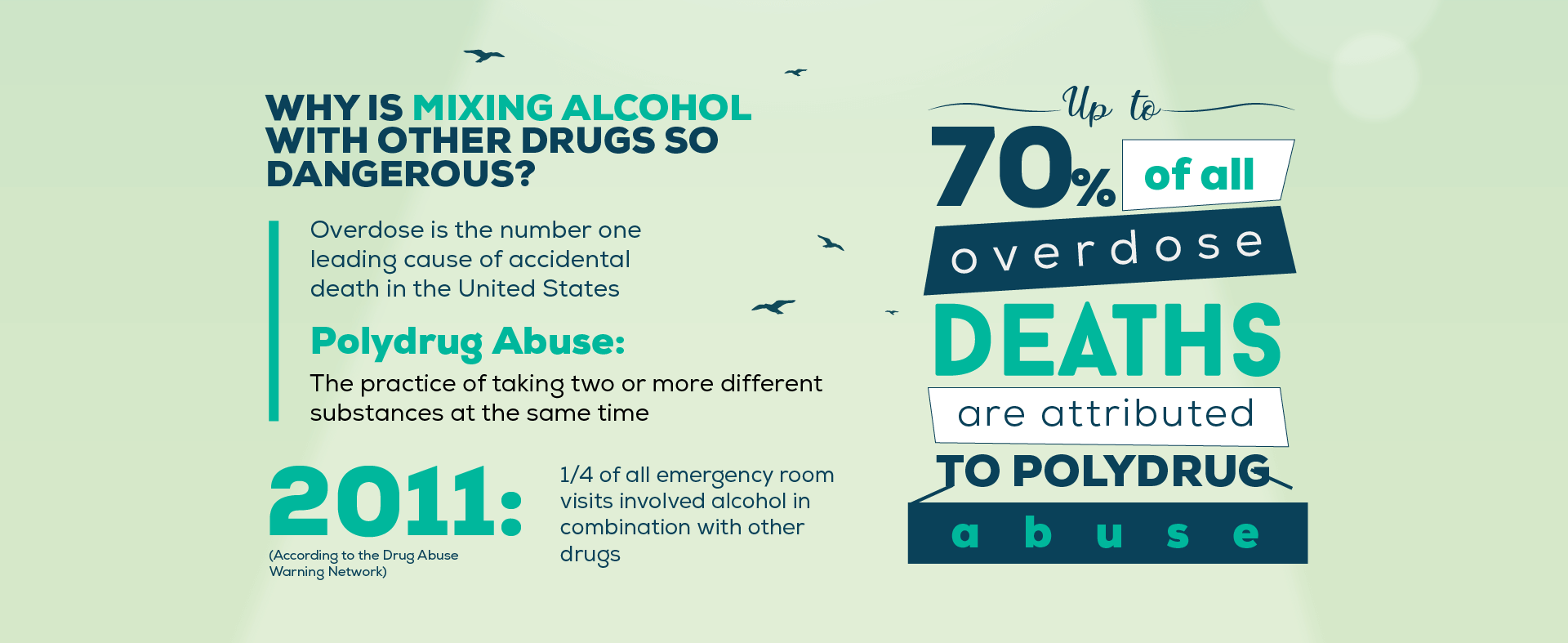
In 2011, a quarter of all emergency room visits involved alcohol in combination with other drugs, according to the Drug Abuse Warning Network. Even more alarming, up to 70% of all overdose deaths are attributed to polydrug abuse - the practice of taking two or more different substances at the same time. Scariest of all, some of those deaths were entirely accidental, such an aging individual who decides to have a few beers after taking a common heart medication.
Overdose is the number one leading cause of accidental death in the United States, and a great many of those deaths could be prevented if the general public understood the dangers of mixing alcohol with other drugs. This does not only apply to illicit drugs; many emergency rooms visits for overdose occur because people unwittingly mixed alcohol with seemingly harmless over-the-counter medications recommended by doctors. Do you know which medications are safe to take with a glass or two of wine? If not, your lack of knowledge could be disastrous in the future.
In this article we'll discuss the dangers of mixing alcohol with other substances and what these hazardous combinations can do to your body.
Why Is Mixing Alcohol with Other Drugs so Dangerous?
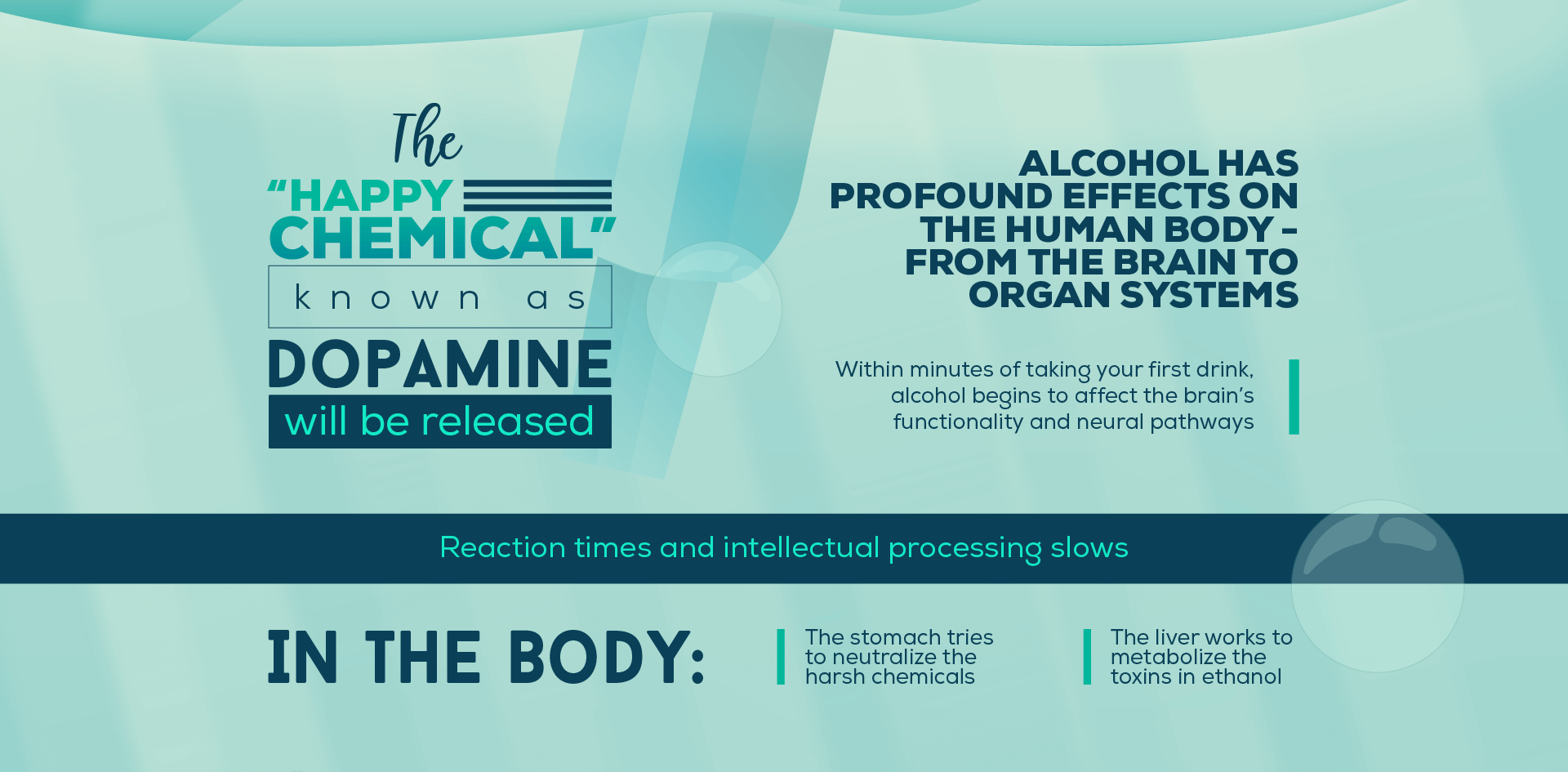
Alcohol, in and of itself, exhibits pronounced effects on the human body, from the brain to organ systems. Within minutes of taking your first drink, alcohol will begin to affect your brain's functionality and neural pathways. The "happy chemical" known as dopamine will be released, causing a feeling of euphoria, as reaction times and intellectual processing slow. In the body, the stomach will be doing its best to neutralize the harsh chemicals as they blaze their way through your system, and the liver will go into overtime in an attempt to metabolize the toxins in ethanol. All of this happens with alcohol consumption alone.
Now, add in more chemicals and side effects from another drug or medication, and all of those reactions are amplified, along with added mental and physiological changes from the other substances. Your brain will be challenged to manage the multiple neural messages it is receiving, and may lose the ability to continue juggling the millions of processes it has to control, such as equilibrium, consciousness, heart rate, or just breathing. At the same time, your stomach, liver, and intestines will be inundated with chemicals and toxins to process and metabolize in an attempt to neutralize the various poisons running through them.
Are you starting to see the problem? Even mild pain relievers like Tylenol and Advil come with a set of ingredients that may not be easy for your body to process if it is already bogged down by the effects of alcohol. The risk of overdose or alcohol poisoning is significantly higher once additional substances are added to the mix, even if those substances seem like innocuous medications.
Who Is at the Most Risk from Combining Alcohol with Other Substances?
Polydrug abuse is dangerous for anyone. No one is immune to the potentially disastrous effects of combining medications or illicit drugs with alcohol, but it does present a greater risk for some people than for others.
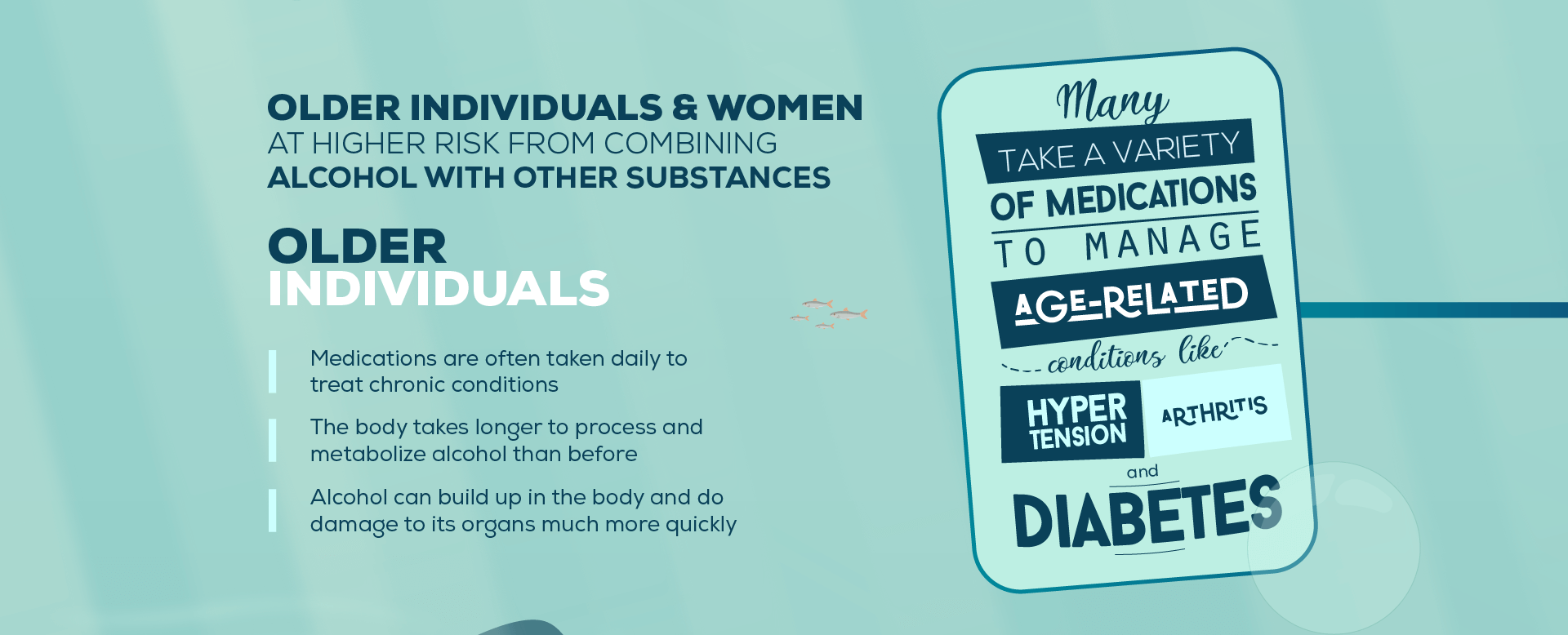
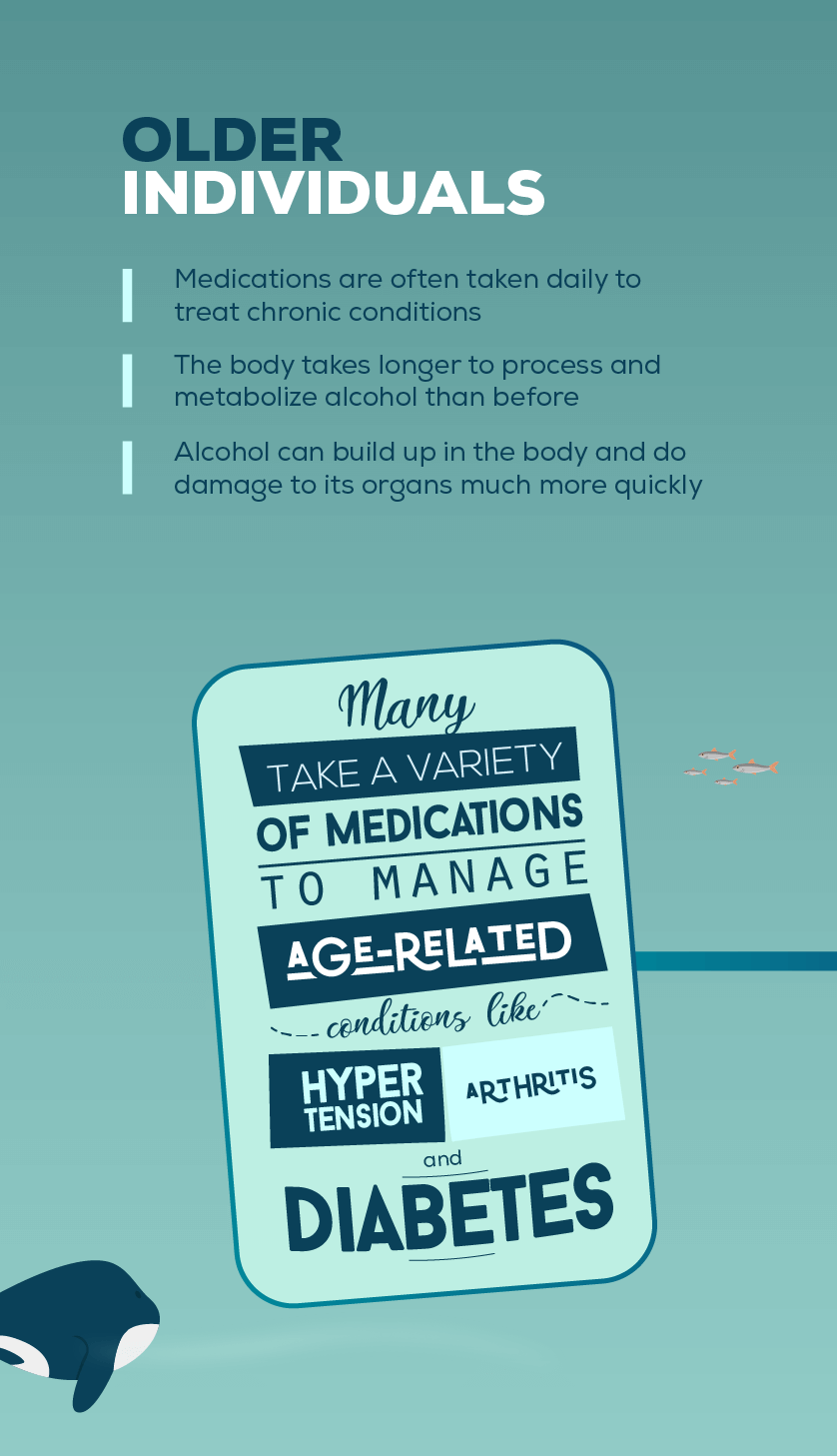
Aged Individuals
Men and women of advanced age are most at risk from mixing drugs and alcohol. For one thing, most older individuals take a variety of medications to manage age-related conditions like hypertension, arthritis, and diabetes. Since these medications are taken daily to treat chronic conditions, any drink that the individual has will present issues with mixing substances.
Another problem is that the body no longer processes and metabolizes alcohol at the same rate as it grows older. The older the individual, the less alcohol they can metabolize at any given time. Because of this, alcohol can build up in the body and do damage to its organs much more quickly in an older individual. This phenomenon also leads to a higher likelihood of overdose or alcohol poisoning if the individual mixes alcohol with other medications or substances.
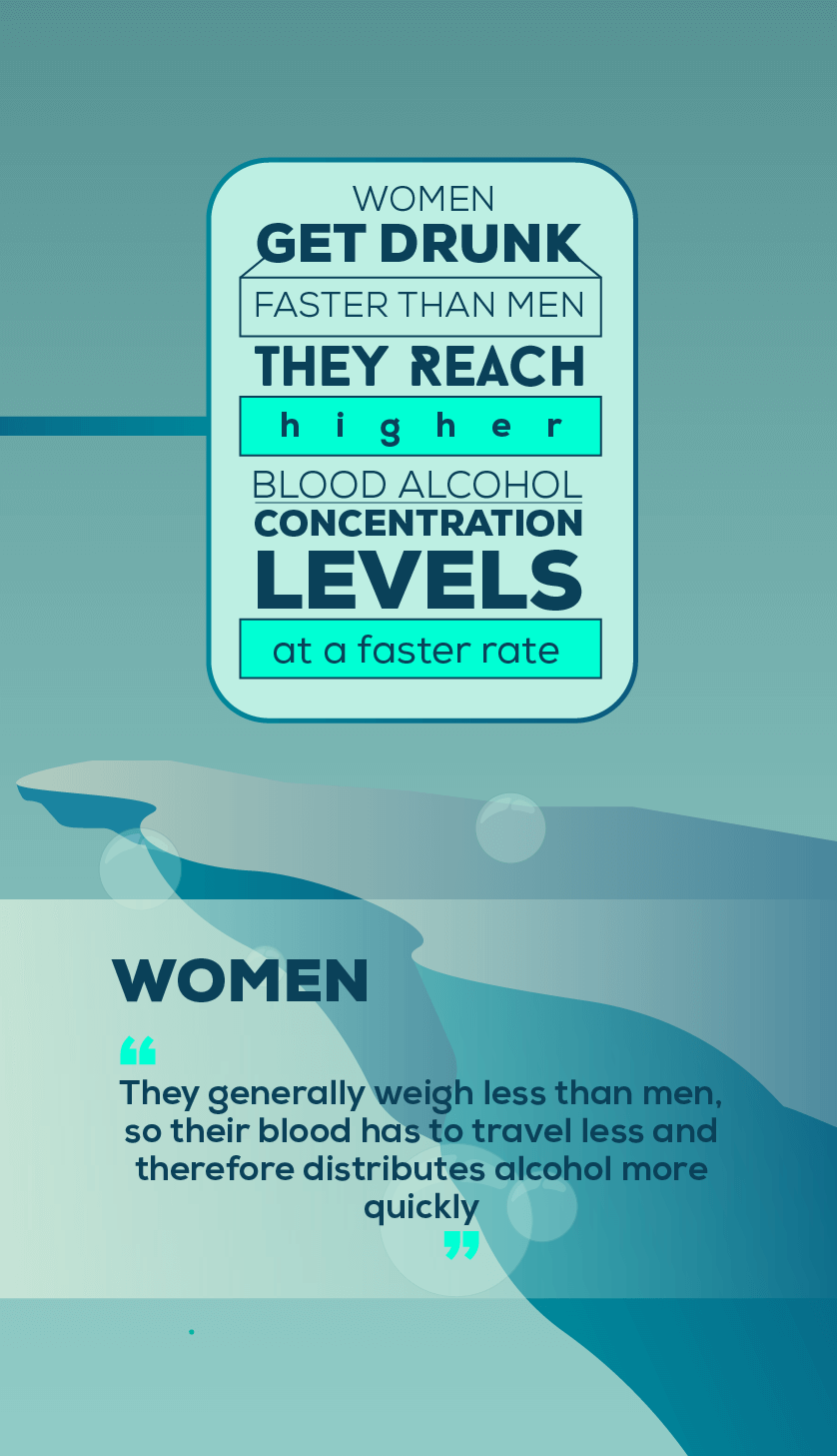
Women
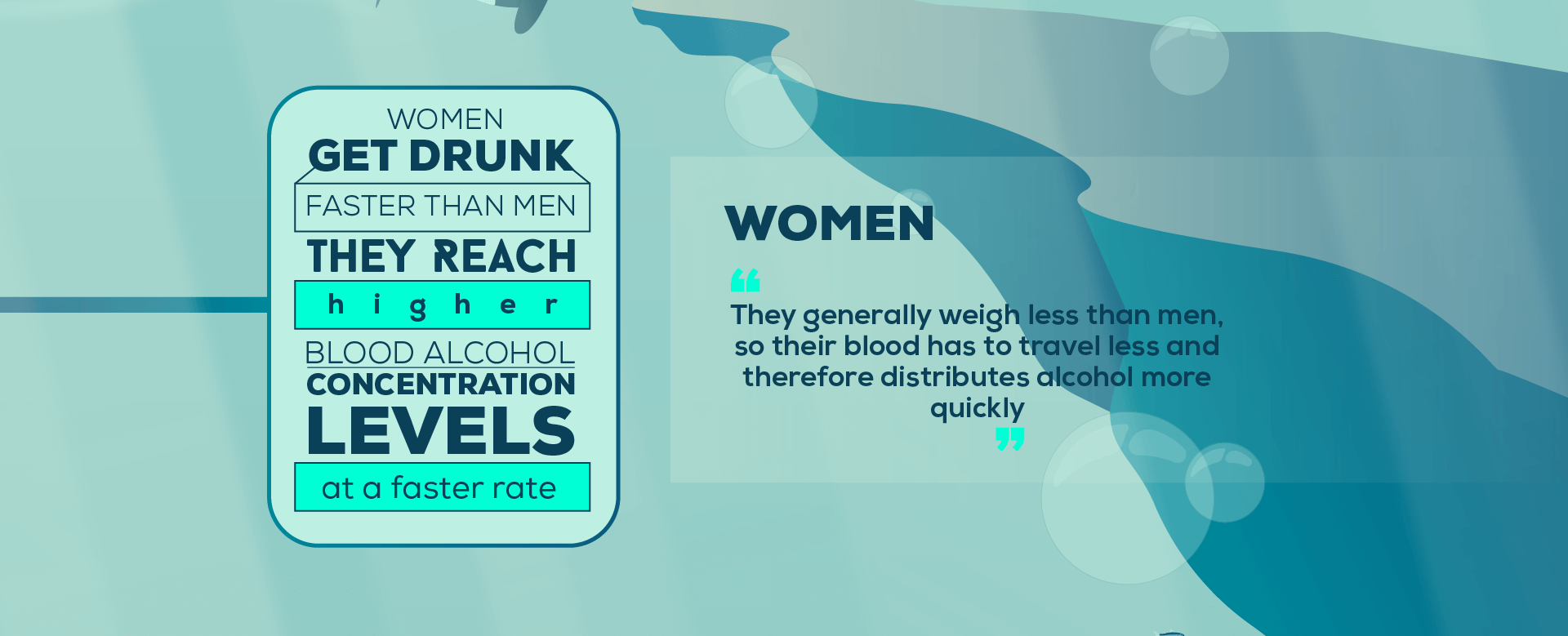
Like it or not, women get drunker faster. Not only do women generally weigh less than men, meaning their blood has less ground to travel and therefore distributes alcohol more quickly; it also has to do with body composition.
Since women's bodies have a higher fat to water ratio than men as a rule, they reach a higher blood alcohol concentration at a faster rate, even if they are the same size and weight as a man drinking the same amount. This means that women also metabolize and absorb other substances more quickly, making women more vulnerable to overdose than men, especially when combining multiple substances.
1. Combining Different Types of Alcohol
"Beer before liquor, never been sicker."
We've all heard that one, right? Although this does not technically count as mixing substances, it is something to consider when you head out for a night out on the town. The truth is, mixing alcohols does not actually make you sick or worsen the hangover. It's all about the total amount of alcohol you consume and the rate at which you consume it.
Since strong liquor like whiskey, vodka, and rum have a much higher alcohol content than drinks like beer or wine, people generally feel their effects much faster. By drinking the hard stuff first and then moving on to a weaker drink like beer, you are slowing down your rate of alcohol intake and are more likely to feel the effects of the drinks you take in and stop when necessary. This type of transition also gives your body more time to metabolize the drinks as they come.
If you start slow with a few beers, on the other hand, and then ramp up the alcohol intake and start to take shots, you will likely take in too much alcohol too quickly, not realizing the effects of the hard liquor you are drinking until it's too late. At the same time, your body was metabolizing weaker beverages when you suddenly threw hard liquor into the mix, inundating the system with more liquor than it was previously prepared to handle. This effect can lead to vomiting and a terrible hangover because of the ethanol toxins that build up in the system when you drink too much, too fast.
In short, it's the quantity you drink and the rate at which you drink it that matters, not necessarily the types of alcohol you consume.
2. Combining Alcohol with Opioid Painkillers
Opioid painkillers include a wide variety of prescription medications, such as:
- Oxycodone (Oxycontin, Percocet)
- Codeine
- Hydrocodone (Vicodin, Lorcet, Lortab)
- Morphine (Kadian, Avinza)
- Fentanyl
- Demerol
The mixing of alcohol with opioids is responsible for more polydrug overdoses than any other combination of drugs. To say that combining these two classes of substances is dangerous is a vast understatement. The combination is often lethal.
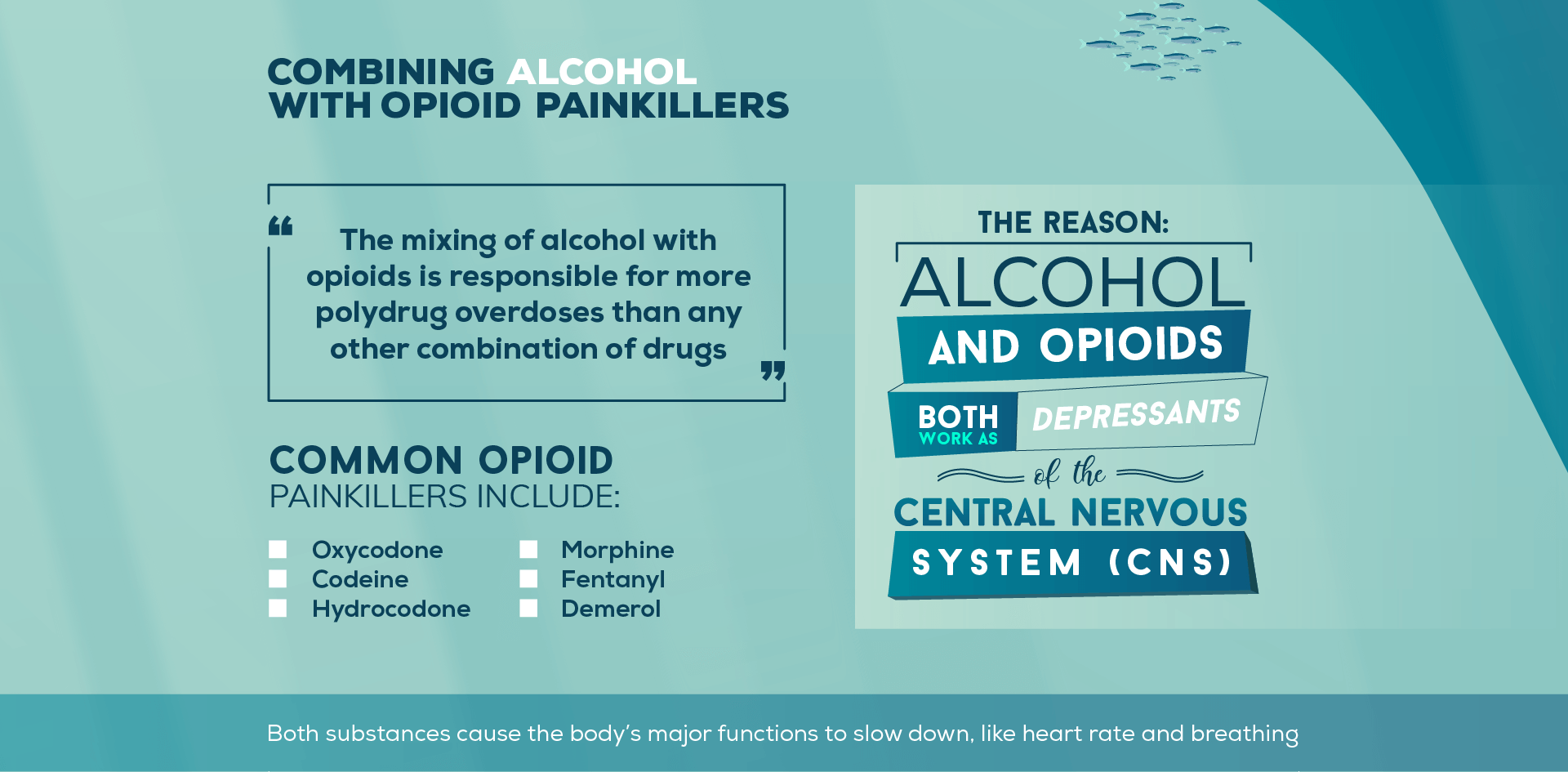
The reason why is because alcohol and opioids both work as depressants of the central nervous system (CNS). Both substances cause the body's major functions to slow down, like heart rate and breathing. One or the other substance might not slow these systems to dangerously low rates, but when they are combined, the body may not be able to control their depressing effects. With a little too much of either substance, the CNS may slow to the point of stopping; in other words, the heart may forget to beat or the lungs may forget to expand and then, it's all over.
Even so much as one beer mixed with opioid painkillers (whether it's prescribed by a doctor or not) puts you at a higher risk for overdose. This is one mistake you might never come back from.
3. Heroin and Alcohol
Heroin is technically another opioid like those medications named above, but its effects can be
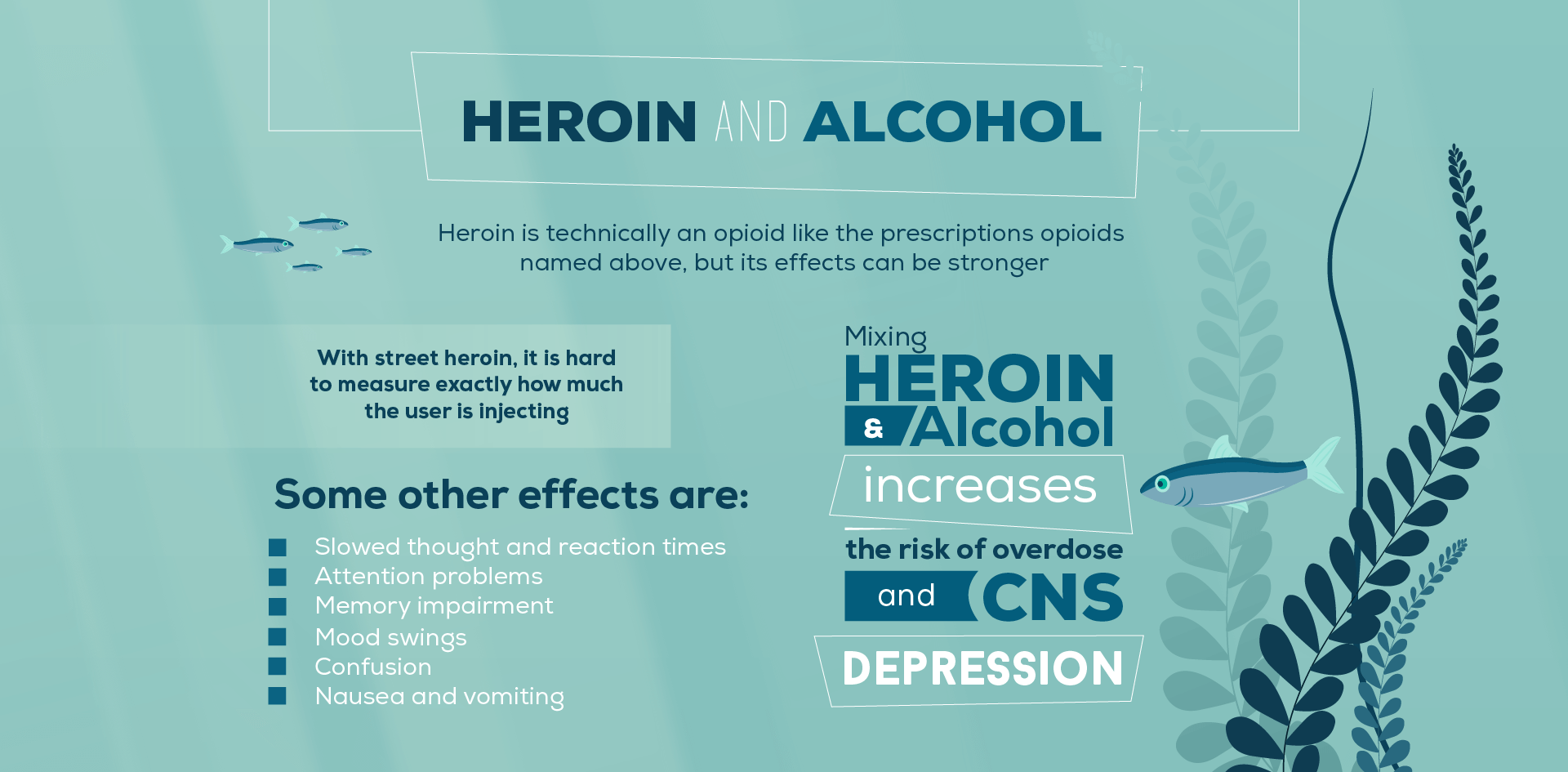

stronger. The same CNS depressing effect occurs when a user mixes alcohol with heroin as when they mix alcohol with opioid painkillers. The only difference is that with street heroin, it is hard to measure exactly how much the user is injecting, so overdose is even more likely. Potential overdose and CNS depression are not the only effects that this deadly combination can have on the human body. Here are some others:
- Slowed thought and reaction times
- Attention problems
- Memory impairment
- Mood swings
- Confusion
- Nausea and vomiting
- Constipation
- Coordination issues
- Slurred speech
- Drowsiness
- Stupor
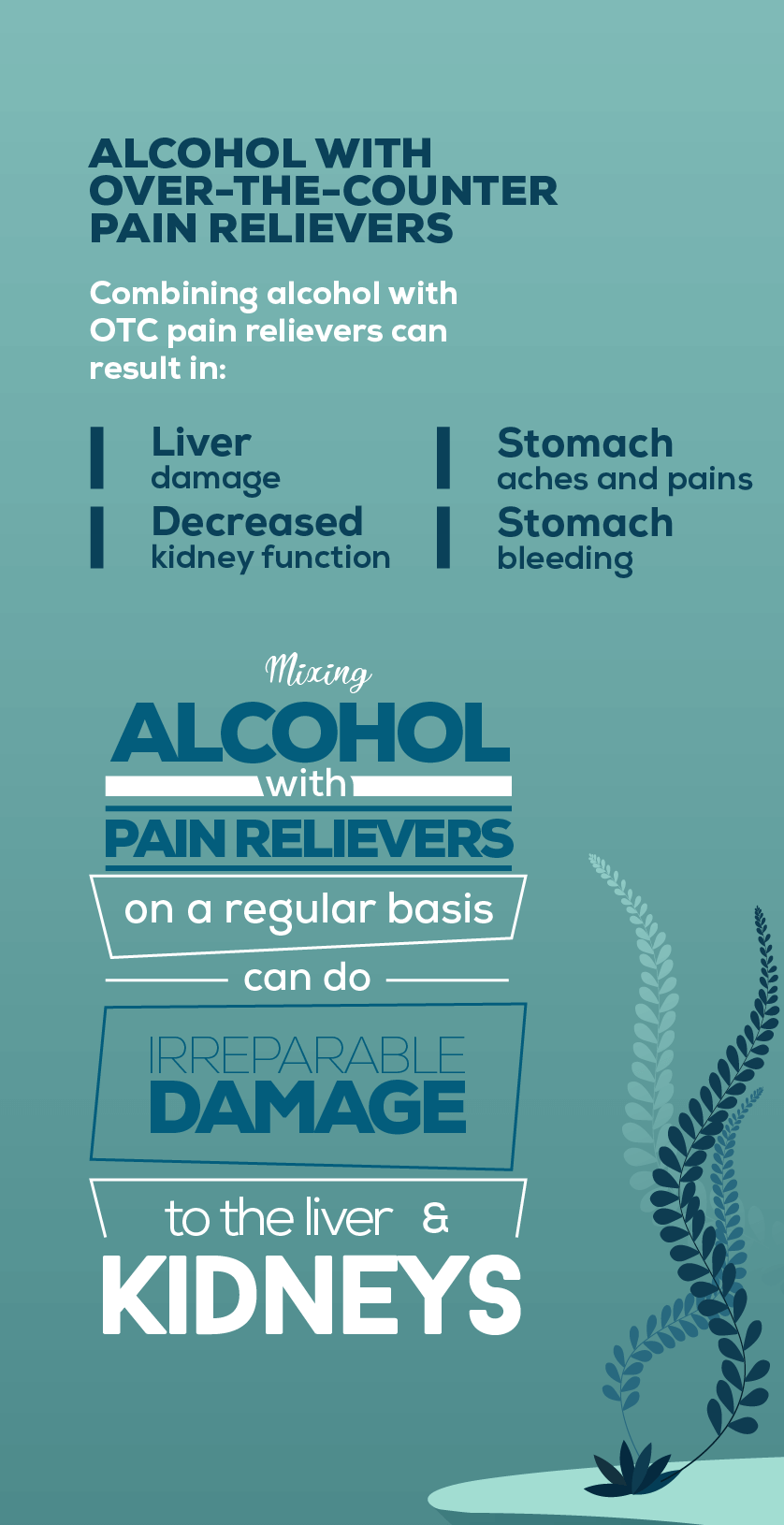
4. Alcohol with Over-the-Counter Pain Relievers
Over-the-counter (OTC) pain relievers are mild analgesics that relieve aches and pains. They are not narcotic and may be purchased without a prescription. These includes medicines like:
- Acetaminophen (Tylenol)
- Ibuprofen (Advil, Motrin)
- Aspirin (Bayer)
- Naproxen (Aleve, Midol)
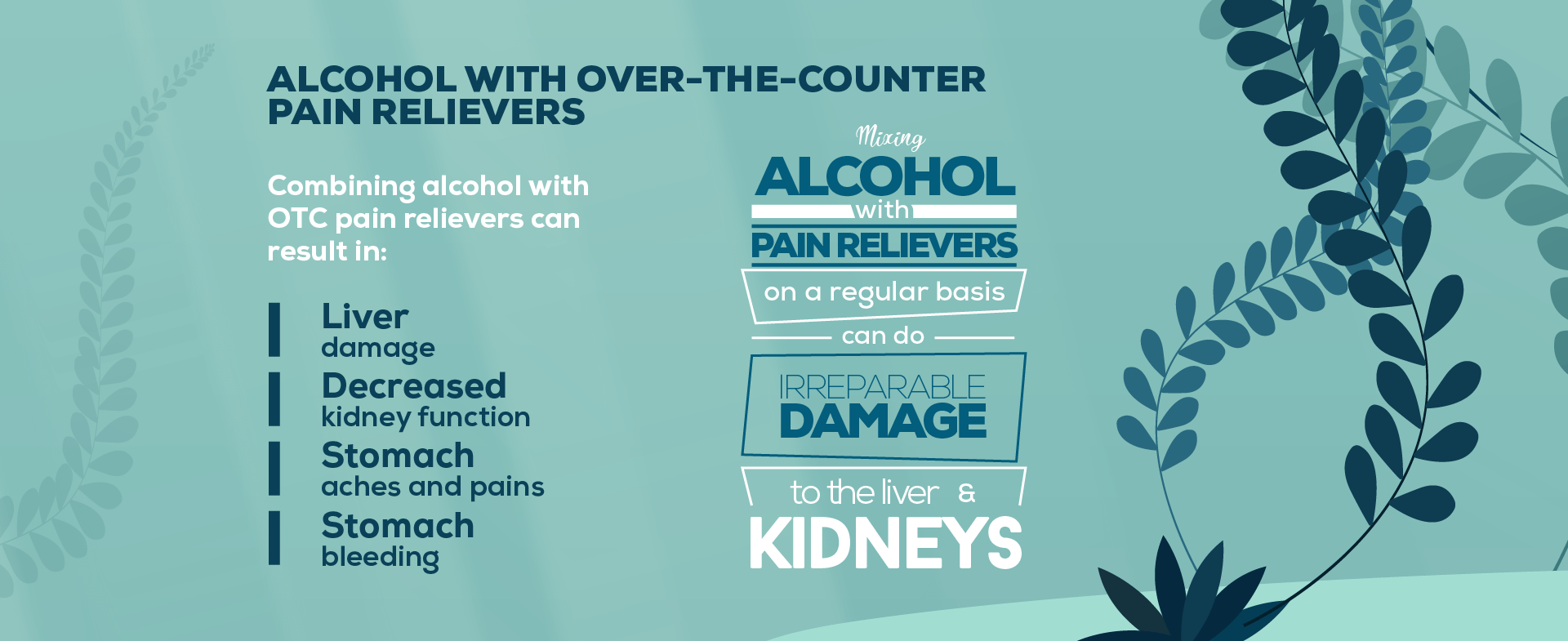
Many people casually take Advil or Tylenol without a second thought, going out to drink with friends as normal. These seemingly harmless pain relievers can actually be difficult for the stomach, liver, and kidneys to process as it is. When alcohol is added to the equation, the organs will be even more taxed and blood alcohol levels will be higher than normal. Combining alcohol with OTC pain relievers can result in:
- Liver damage
- Decreased kidney function
- Stomach aches and pains
- Stomach bleeding
- Ulcers
- Accelerated heart rate
If you mix alcohol with pain relievers on a regular basis, it is likely that you will do irreparable damage to your liver and kidneys. Be mindful when you drink, and always take note when you take even the mildest of pain relievers.
5. Combining Alcohol and Anxiety Medications
There are a wide variety of medications prescribed for anxiety, but for the purposes of this article we'll focus on benzodiazepines and beta blockers. Prescriptions like these can reduce stress, panic attacks, stress-related hypertension, and social anxiety, and so are often taken on a daily basis by the patients that need them. Here are some of the most common anxiety prescriptions:
- Alprazolam (Xanax)
- Lorazepam (Ativan)
- Diazepam (Valium)
- Clonazepam (Klonopin)
- Oxazepam (Serax)
- Chlordiazepoxide (Librium)
- Atenolol (Tenormin)
- Propranolol (Inderal)
Every single one of these prescriptions comes with a clear warning on the label not to mix them with alcohol. This is because of similar double-depressant effects as exhibited by mixing alcohol with opioids.
The problem with daily medications like these is that anyone who takes them on a daily basis should completely abstain from drinking alcohol. This can be difficult for the average person, especially at parties and during holiday festivities. The dangers of mixing alcohol with anxiety medications, however, are very real. Besides the increased risk of overdose, these are some of the potential side effects:
- Severely inhibited cognition and reasoning abilities
- Lack of motor skills and coordination
- Nausea and vomiting
- Increased risk of heart attack, stroke, or seizures
- Psychosis
- Liver and kidney damage
- Increased risk of developing psychological conditions like depression, bipolar disorder, psychotic disorders, or anxiety disorders
6. Mixing Muscle Relaxers and Alcohol
Another CNS depressant, muscle relaxers work by relaxing the CNS and loosening muscle tension, which helps to prevent spasms, spasticity, and back pain. Since it is a CNS depressant, muscle relaxers are dangerous to combine with alcohol; they tend to work together in reducing the functions of the CNS to dangerously low levels. This greatly increases the risk of overdose. Other side effects of mixing alcohol with muscle relaxers include:
- Drowsiness
- Impaired motor control
- Unusual behavior
- Decreased memory retention
- Dizziness
- Higher risk of seizures
- Slowed or difficulty breathing
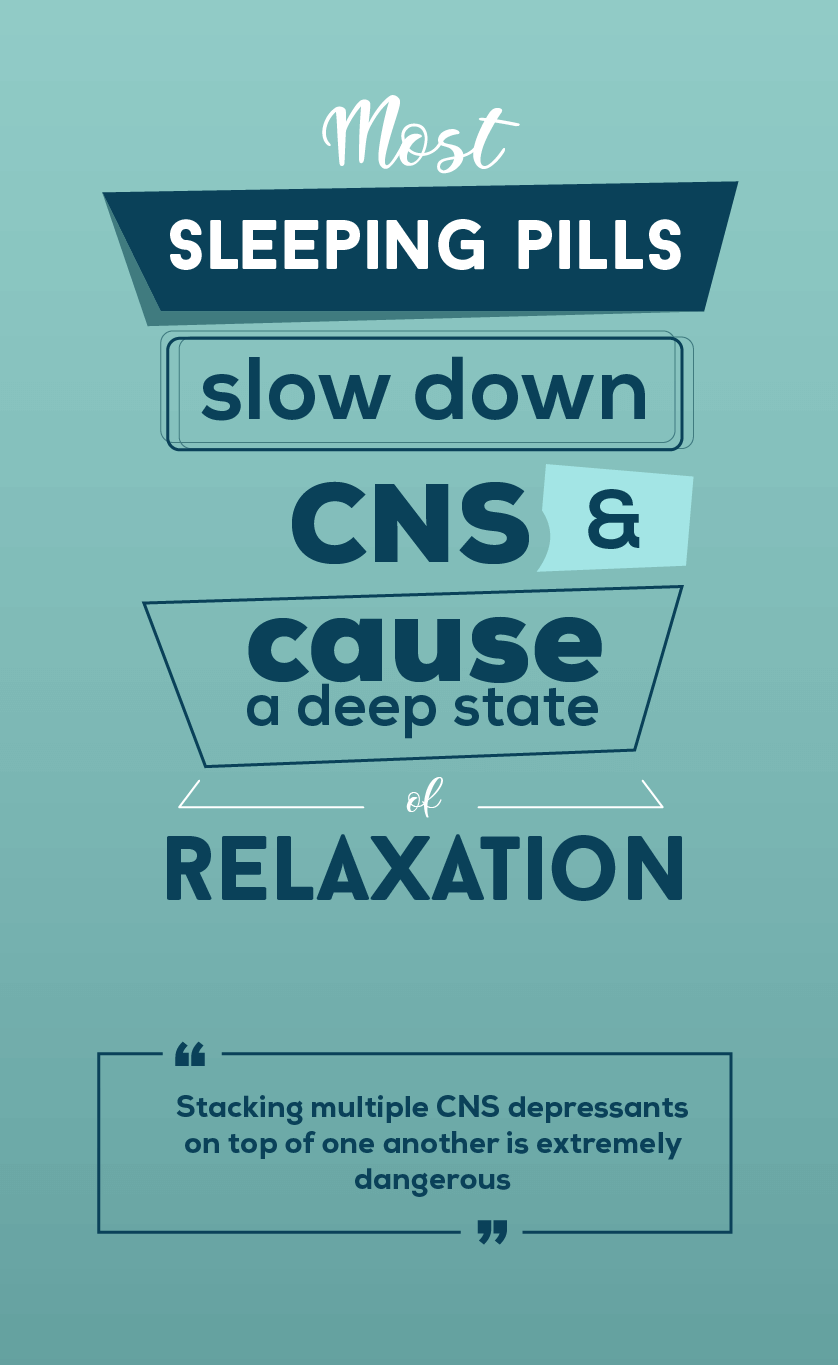
7. Mixing Alcohol with Sleep Aids
Like opioids, sleep aids are one of the most dangerous substances you can mix with alcohol. Most sleeping pills work by slowing down the CNS and causing a deep state of relaxation. The most popular brands of sleep aids are:
- Sonata
- Rozerem
- Belsomra
- Ambien
- Lunesta
- Prosom
- Restoril
- Sominex
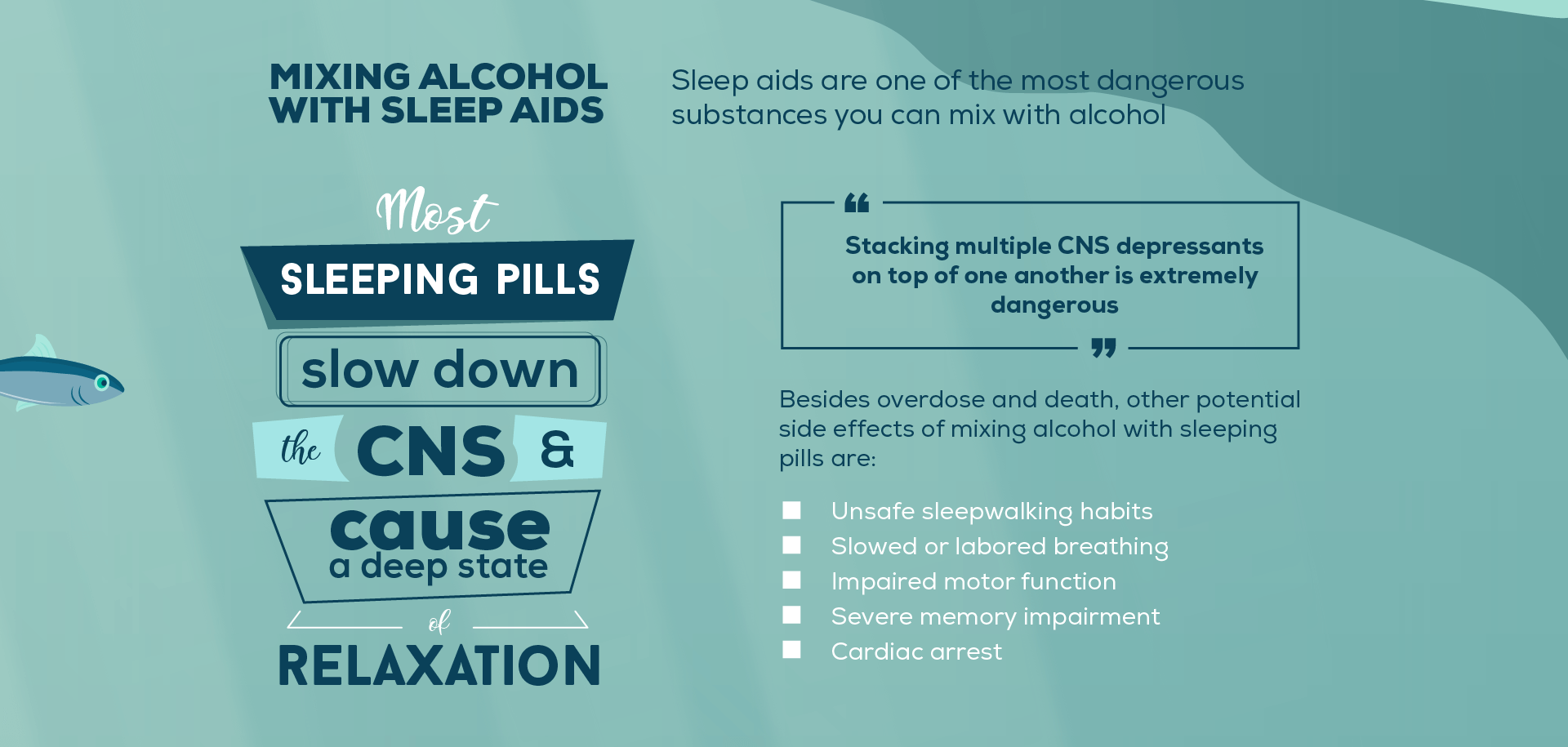
Once again, stacking multiple CNS depressants on top of one another is extremely dangerous. Besides overdose and death, other potential side effects of mixing alcohol with sleeping pills are:
- Unsafe sleepwalking habits
- Slowed or labored breathing
- Impaired motor function
- Severe memory impairment
- Cardiac arrest
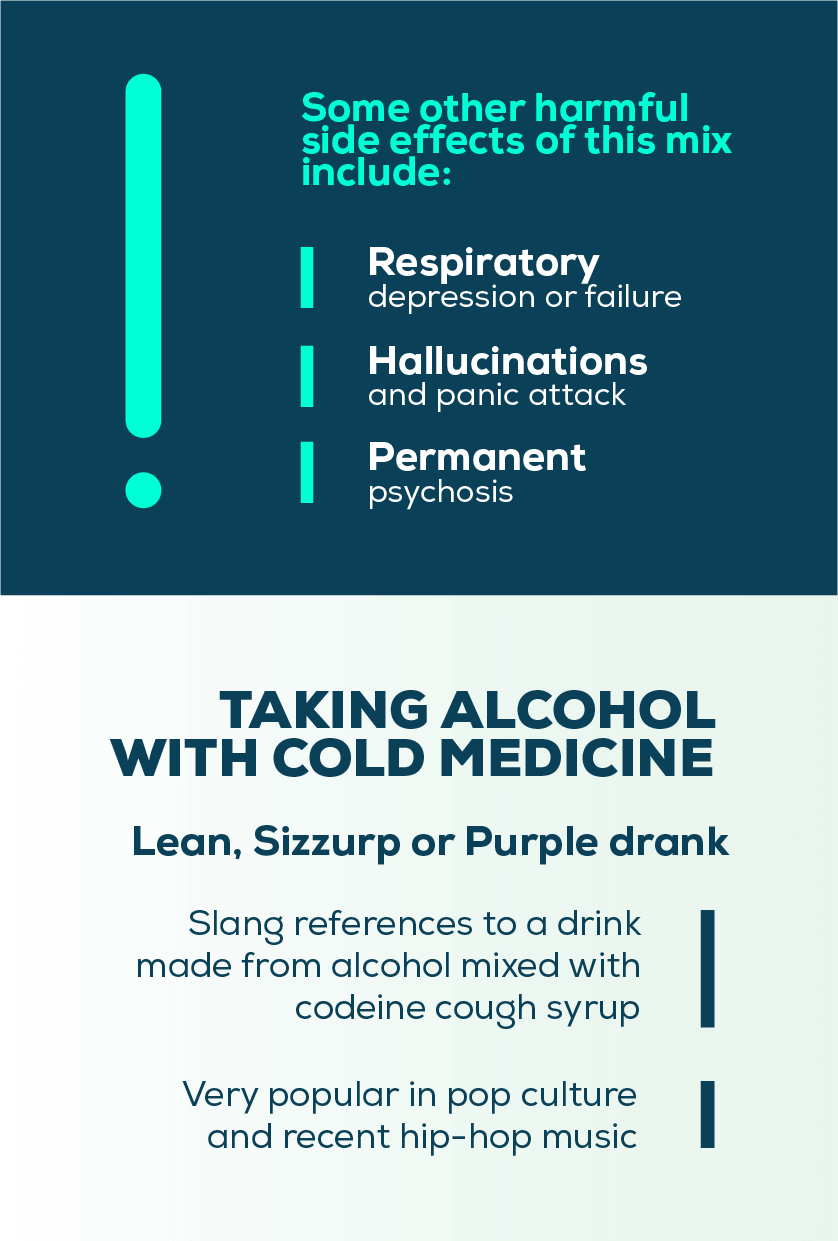
8. Taking Alcohol with Cold Medicine
If you've listened to hip hop music over the years, it's likely that you've heard mention of "lean", "sizzurp" or "purple drank". These are slang references to a drink concocted of alcohol mixed with codeine cough syrup. This combination is a dangerous mix, made even more hazardous by its popularity in pop culture.
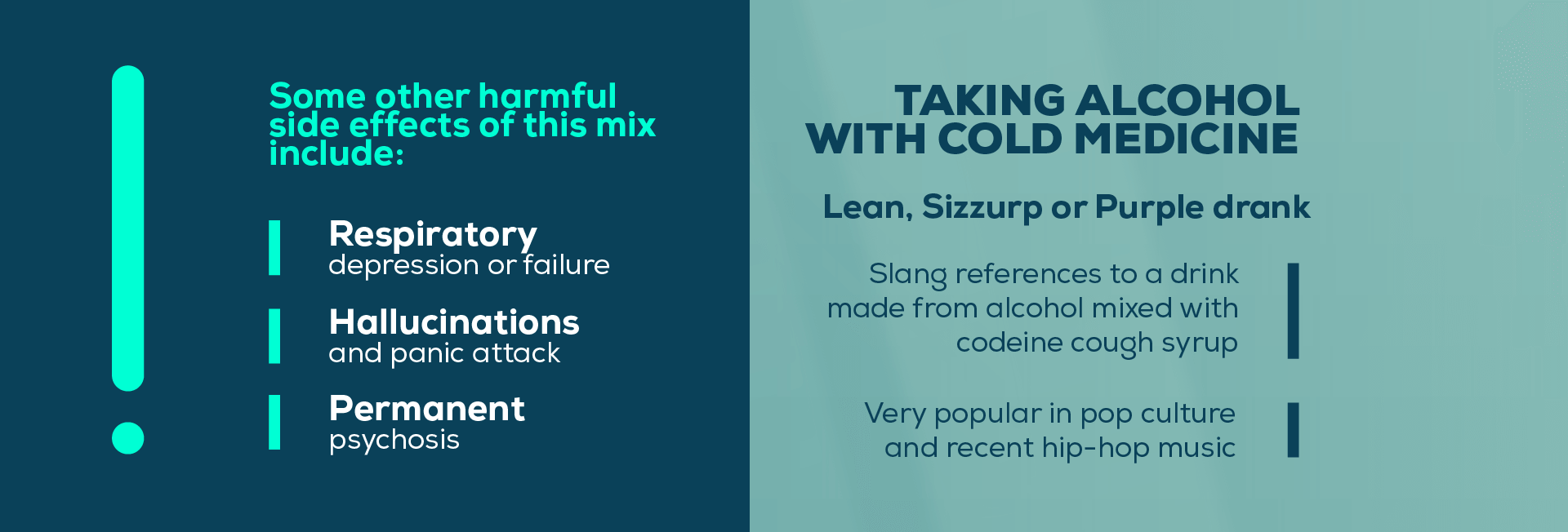
Although the effects of codeine are much stronger, even mixing alcohol with OTC cold medicines like Robitussin or Dayquil is hard on the brain and body. For one thing, cough syrup (whether it contains codeine or not) can be a depressant to the CNS. If the syrup contains codeine or dextromethorphan (DMX), it may also affect brain functioning, especially in high doses. Mixing either of these substances with alcohol presents a high risk of overdose. Some other harmful side effects include:
- Respiratory depression or failure
- Hallucinations and panic attack
- Brain lesions leading to permanent behavioral changes
- Epilepsy
- Permanent psychosis
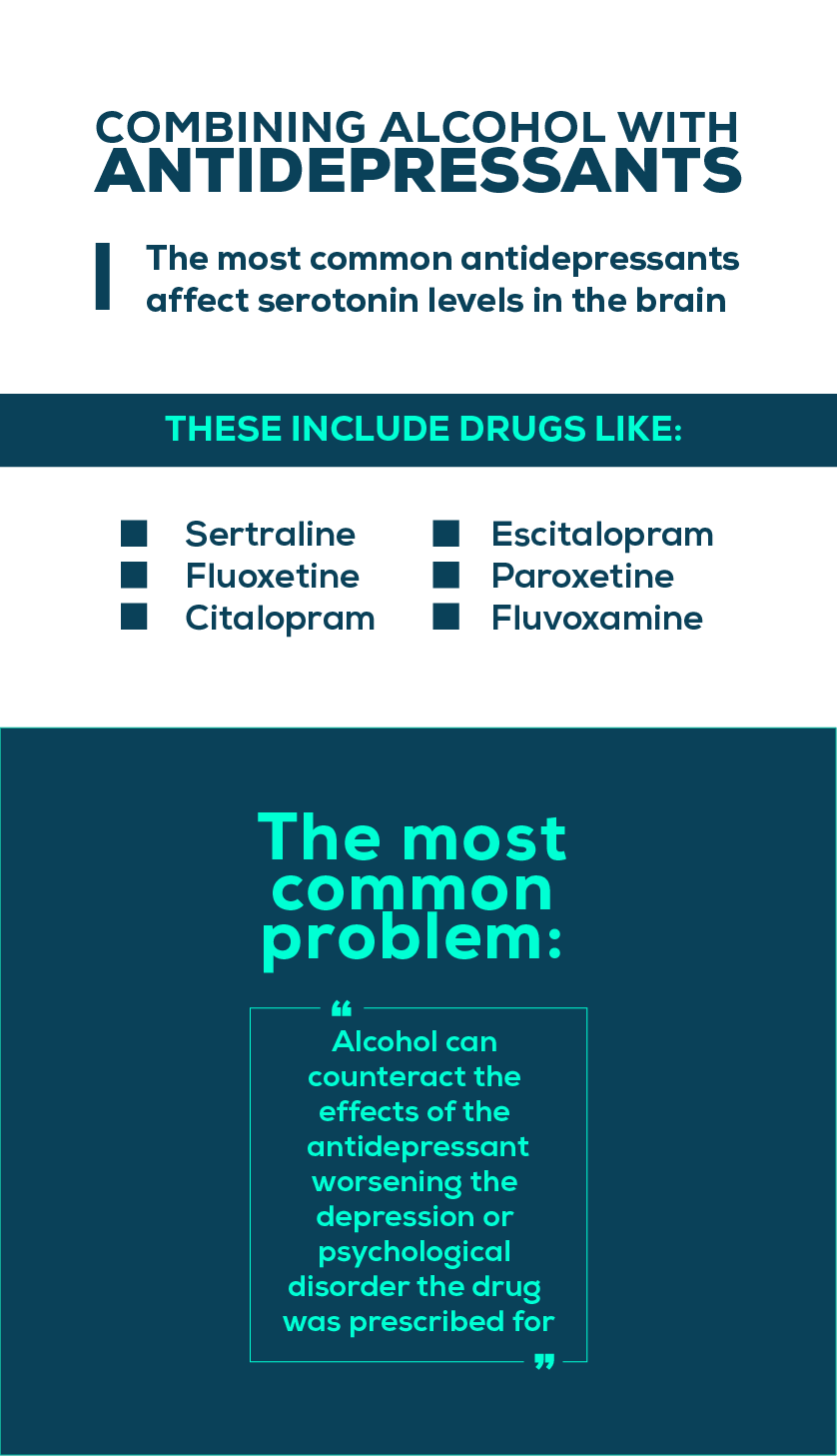
9. Combining Alcohol with Antidepressants
The most common antidepressants affect serotonin levels in the brain and are classified as "selective serotonin reuptake inhibitors (SSRIs)". These include drugs like:
- Sertraline (Zoloft)
- Fluoxetine (Prozac, Sarafem)
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Paroxetine (Paxil, Pexeva, Brisdelle)
- Fluvoxamine (Luvox)
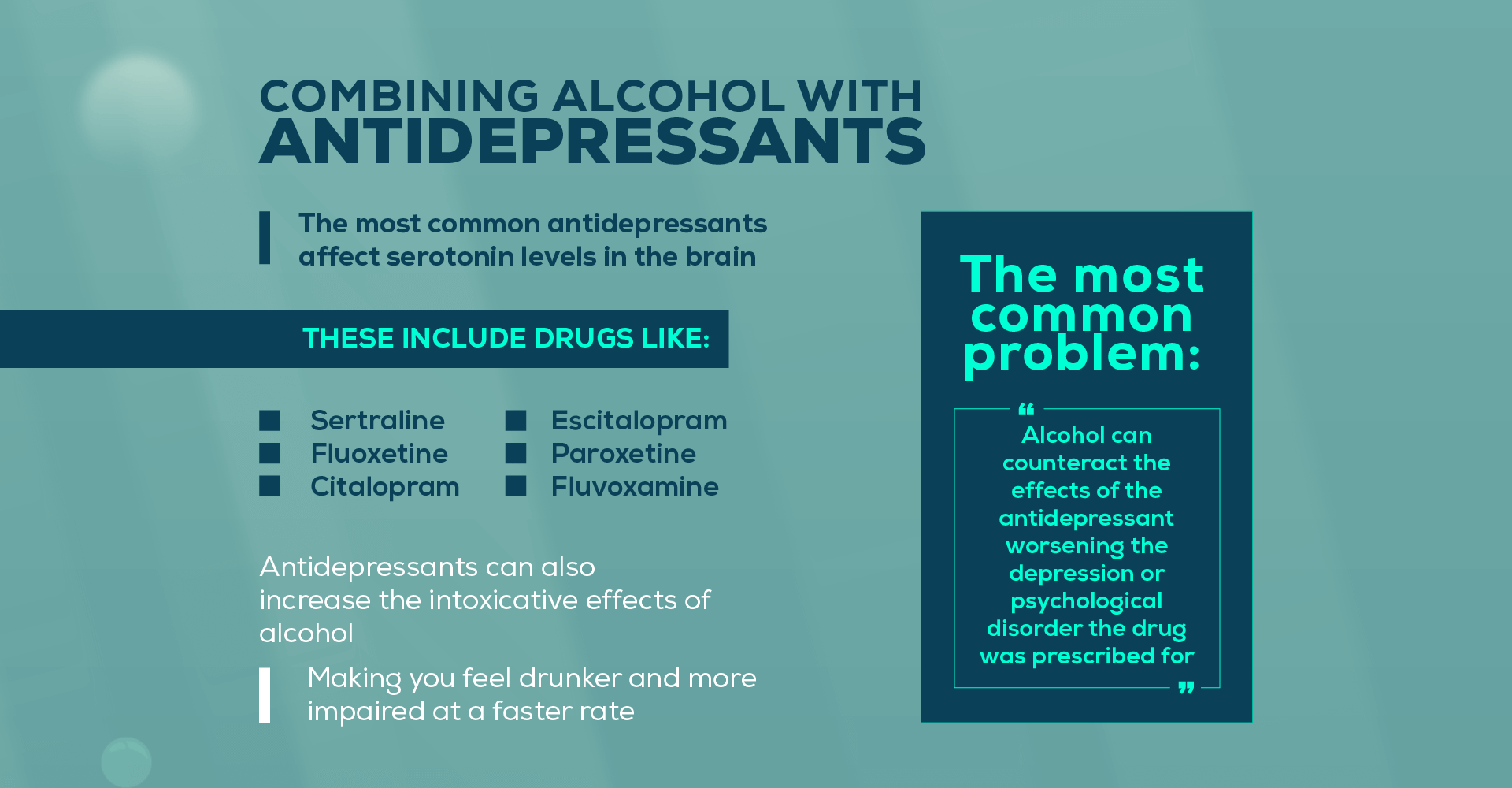
There are other types of antidepressants (such as the dopamine reuptake inhibitor Wellbutrin), but the vast majority of them will have similar effects to SSRIs when combined with alcohol. The most common problem with mixing antidepressants and alcohol is that alcohol can counteract the effects of the antidepressant, exacerbating the depression or psychological disorders that the drugs were prescribed for. Doctors say that in most cases where antidepressants do not work, it has something to do with alcohol consumption. Antidepressants can also increase the intoxicative effects of alcohol, making you feel drunker and more impaired at a faster rate.
10. Combining Alcohol with Mood Stabilizers
Some mood-stabilizing psychiatric medications, like MAOI prescriptions or lithium, can have dangerous - even deadly - reactions with alcohol, so take extra care to never drink alcohol if you take any of these. Some of the potential ramifications of mixing alcohol with mood stabilizers are:
- Dangerous spikes in heart rate
- Upset stomach
- Nausea and vomiting
- Extreme dizziness
- Loss of equilibrium
- Impaired motor control
- Drowsiness
- Tremors
- Blurred vision
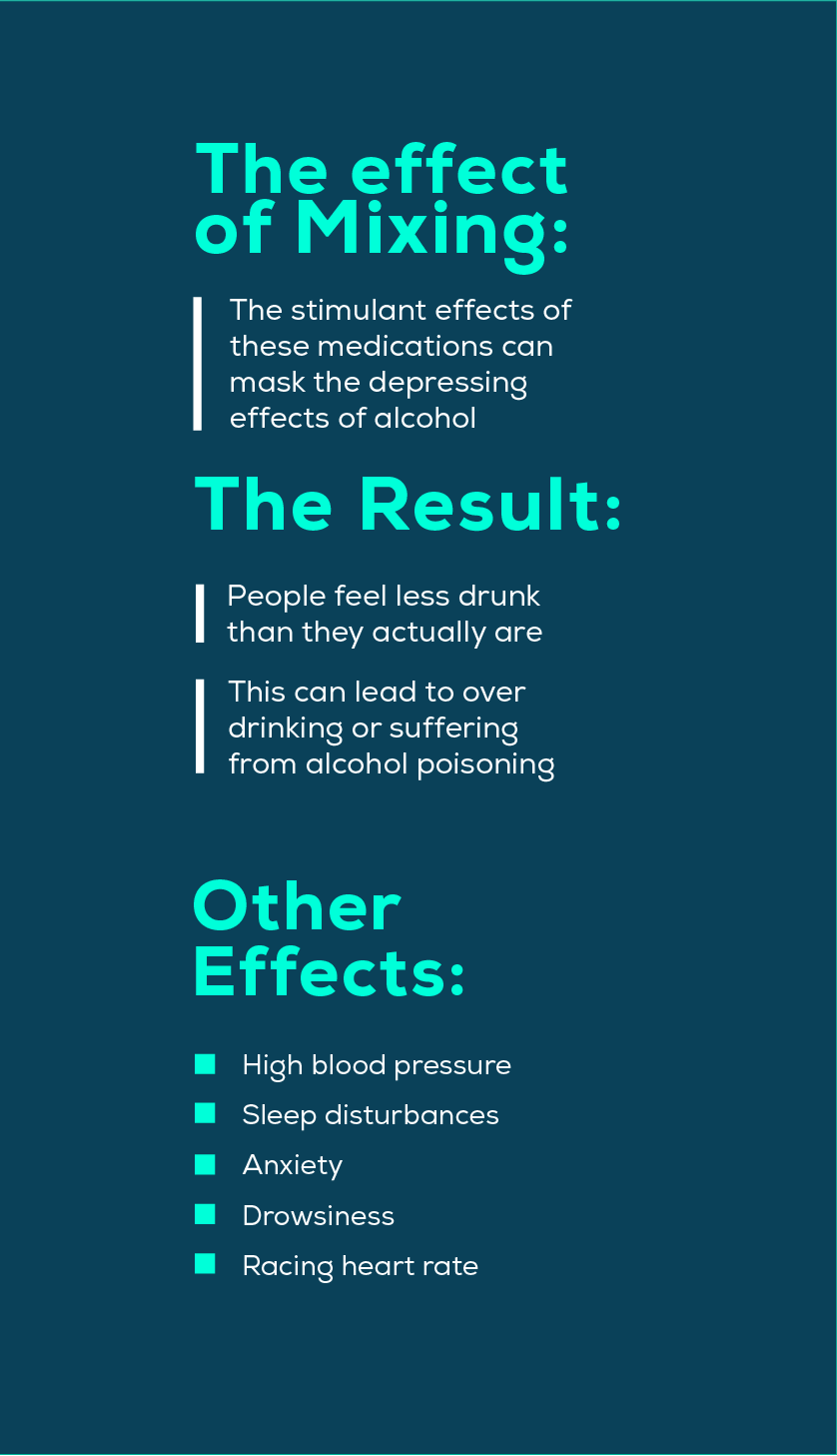
11. Taking Alcohol with Prescription Stimulants
Also called "study aids", prescription stimulants are medications that are usually prescribed for concentration and attention disorders like ADHD and ADD. They include medications like the following:
- Concerta
- Adderall
- Ritalin
- Dexedrine
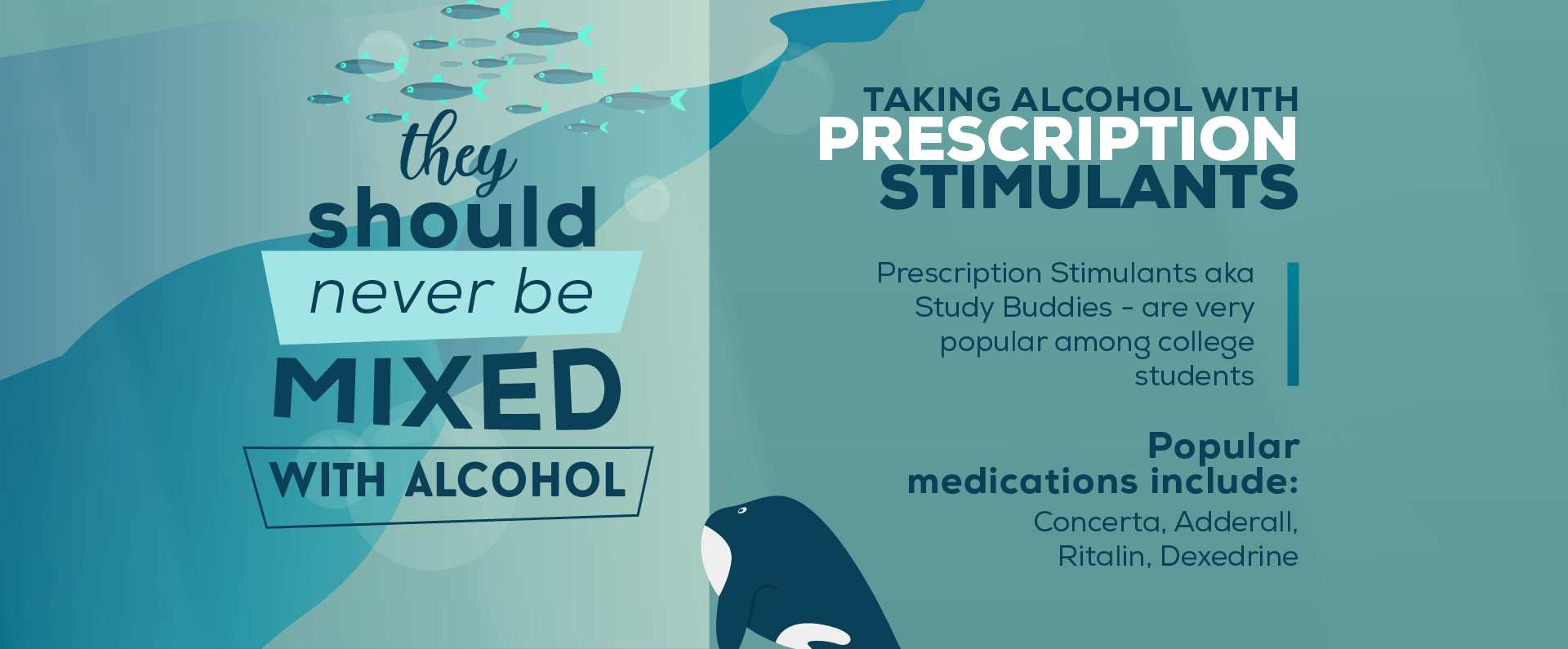
Sometimes they are used by people without attention disorders (or a valid prescription) in order to stay awake and focus on projects for school or work. Others abuse them in order to stay awake longer while partying and clubbing. No matter what you're using them for, prescription stimulants should not be mixed with alcohol.
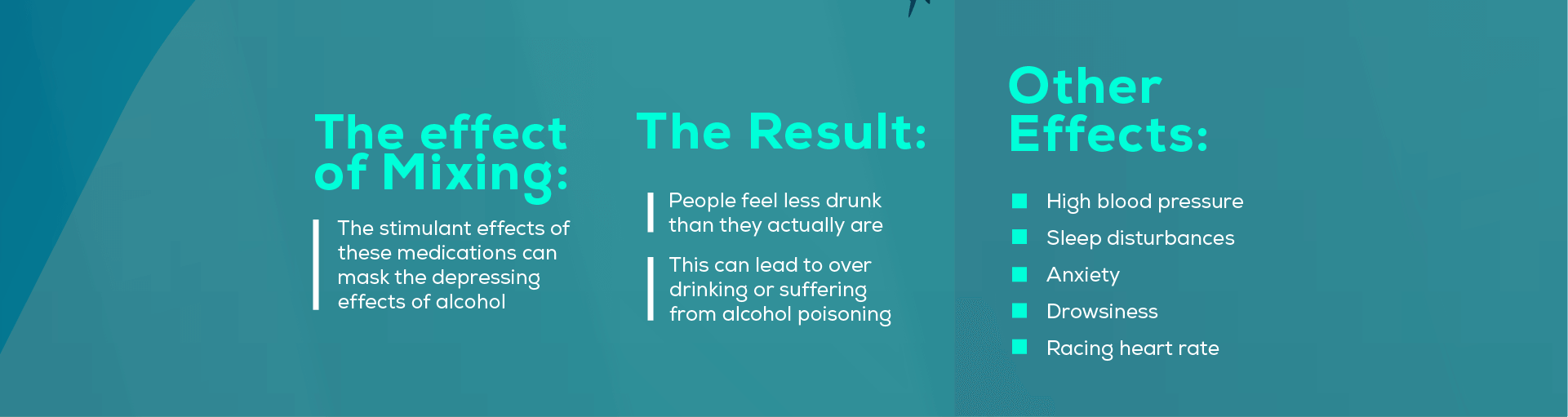
For one thing, the stimulant effects of these medications can mask the depressing effects of alcohol, making you feel less drunk than you actually are. This phenomenon can lead to people over drinking or suffering from alcohol poisoning accidentally. Other potential consequences of mixing prescription stimulants with alcohol are:
- High blood pressure
- Sleep disturbances
- Anxiety
- Drowsiness
- Racing heart rate
12. Combining Alcohol with Diabetes Medication
Drinking alcohol is tricky for anyone who has diabetes, since most types of alcohol contain sugar and carbohydrates. On top of that, alcohol has been shown to have a wide range of interactions with insulin, potentially causing hypoglycemia or hyperglycemia depending on the person.
For those taking diabetes-management medications like metformin or alpha-glucosidase inhibitors, the risks stack even higher when alcohol is involved. Depending on the medication, drinking alcohol may bring sugar levels dangerously low or create dangerous interactions with lactic acid, either of which could lead to hospitalization.
13. Combining Alcohol with Arthritis Medications
Although it is not prohibited by all doctors, most recommend that patients abstain from drinking alcohol while taking arthritis medications like methotrexate due to these reasons:
- Combining alcohol with methotrexate can cause liver damage.
- Drinking alcohol can skew arthritis test results at the doctor's office.
- Alcohol can exacerbate other arthritis-related conditions like fibromyalgia and osteoporosis.
14. Mixing Alcohol and Cholesterol Medications
Having a glass of wine while taking cholesterol medications may not do any immediate damage, although you should always consult your doctor regarding your specific case. That being said, heavy drinkers who take cholesterol medications like statins and bile acid sequestrants are at risk. If you have more than one drink per day while taking cholesterol medications, you may be increasing your risk of developing the following problems:
- Liver damage
- Increased occurrences of medication side effects
- Decreased effectiveness of cholesterol medications
If you have a moderate to heavy drinking habit, it's advisable to consult your doctor before taking cholesterol medications.
15. Combining Alcohol with Heart Medications
Alcohol by itself can affect the heart rate and blood pressure. For that reason alone, people with heart problems are advised to avoid alcohol. If you're taking heart medications at the same time, however, the consequences can be dire indeed. Since heart medications come in several different forms, we'll go over some of the most common types and their potential interactions with alcohol:
- Isosorbide nitroglycerine (Isordil) for heart disease - can cause sudden changes in blood pressure, dizziness, and fainting when mixed with alcohol.
- Warfarin (Coumadin) for blood clots - may cause internal bleeding, strokes, or heart attack when mixed with alcohol.
- Medications to treat high blood pressure (Accupril, Calan, Lorpressor, etc) - can cause dizziness, fainting, or heart arrhythmia when mixed with alcohol.
16. Combining Alcohol with Allergy Medications
Some allergy medications have more adverse interactions with alcohol than others. The general rule is that if the allergy medication can make you drowsy, like Benadryl, it should never be mixed with alcohol for the double CNS-depressing effect the two substances can have.
Non-drowsy antihistamines like Claritin or Allegra, on the other hand, may be safe to take with one or two drinks, although you would be well-advised to ask your doctor before trying it. Heavy drinking while taking any allergy medication, however, could cause stomach pain, cramps, and vomiting, so keep this combination to a minimum.
17. Mixing Alcohol and Weed (aka Being Crossfaded)
Marijuana combined with alcohol, also known as crossfading, is one of the most common polydrug addictions. Since both are seen as "soft" drugs, people rarely recognize the risks of sitting back to drink a few margaritas and smoke a joint, but the danger is real.
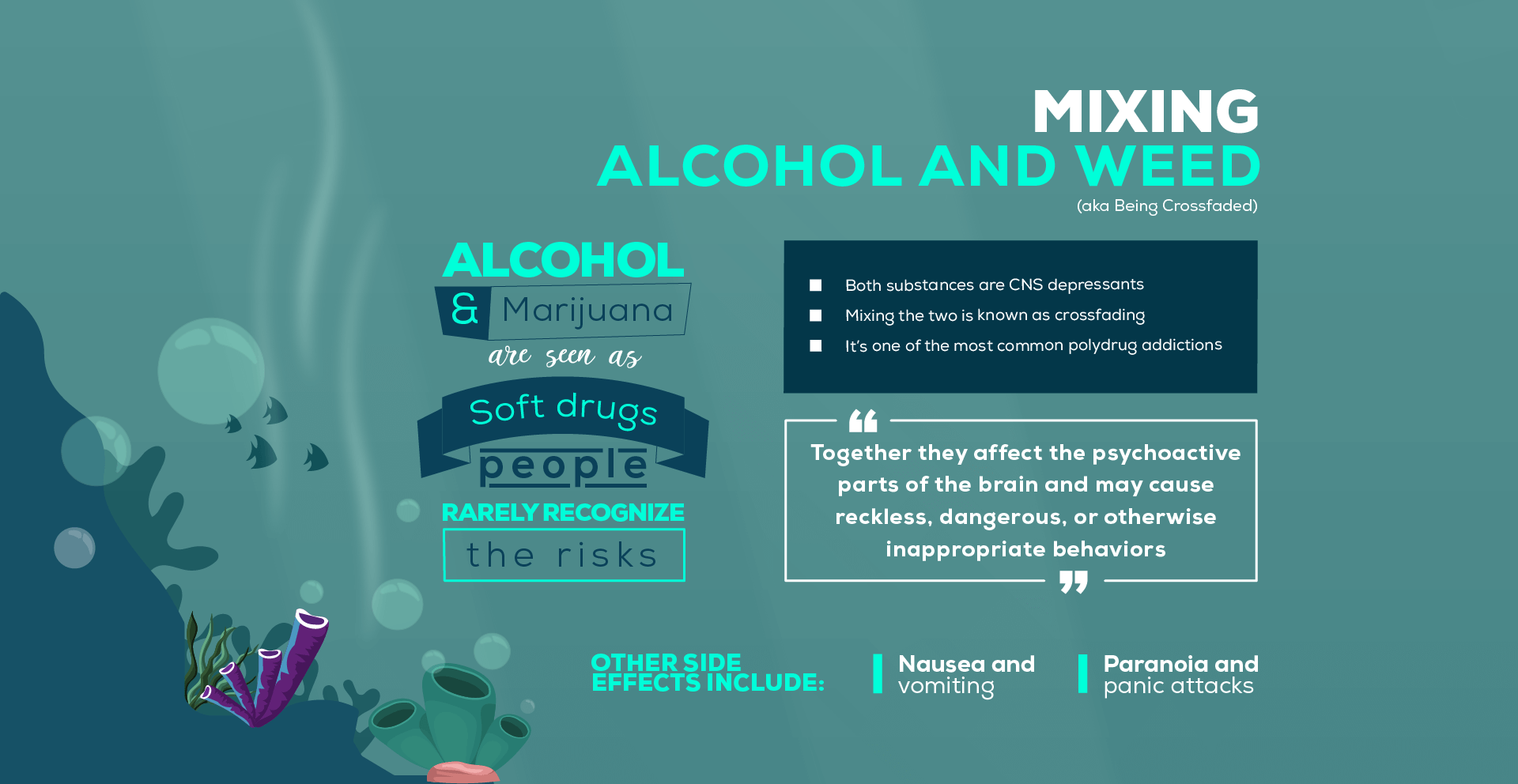
Both of these substances are CNS depressants and can slow the breathing and heart rate to lower levels when combined. Although weed presents less risk of overdose than opioids or other illicit substances, it can lead to higher risk of alcohol poisoning when combined with alcohol. First of all, levels of both THC and ethanol will be higher when the two or mixed than when they are consumed separately. Marijuana also has the effect of inhibiting the vomit reflex, making it less likely that people will vomit when they drink an excess of alcohol. Vomiting is your body's way of purging out toxic substances, so if you are unable to vomit excess alcohol, it stays in your system and is more likely to cause alcohol poisoning.
You may also notice a marked decrease in decision-making abilities if you mix weed and alcohol. These two substances together affect the psychoactive parts of the brain and may cause reckless, dangerous, or otherwise inappropriate behavior. Some other unfortunate side effects of mixing these two substances include:
- Nausea and vomiting
- Paranoia and panic attacks
- Anxiety
- Impaired processing and decision-making abilities
18. Combining Alcohol with Cocaine & Other Illicit Stimulants
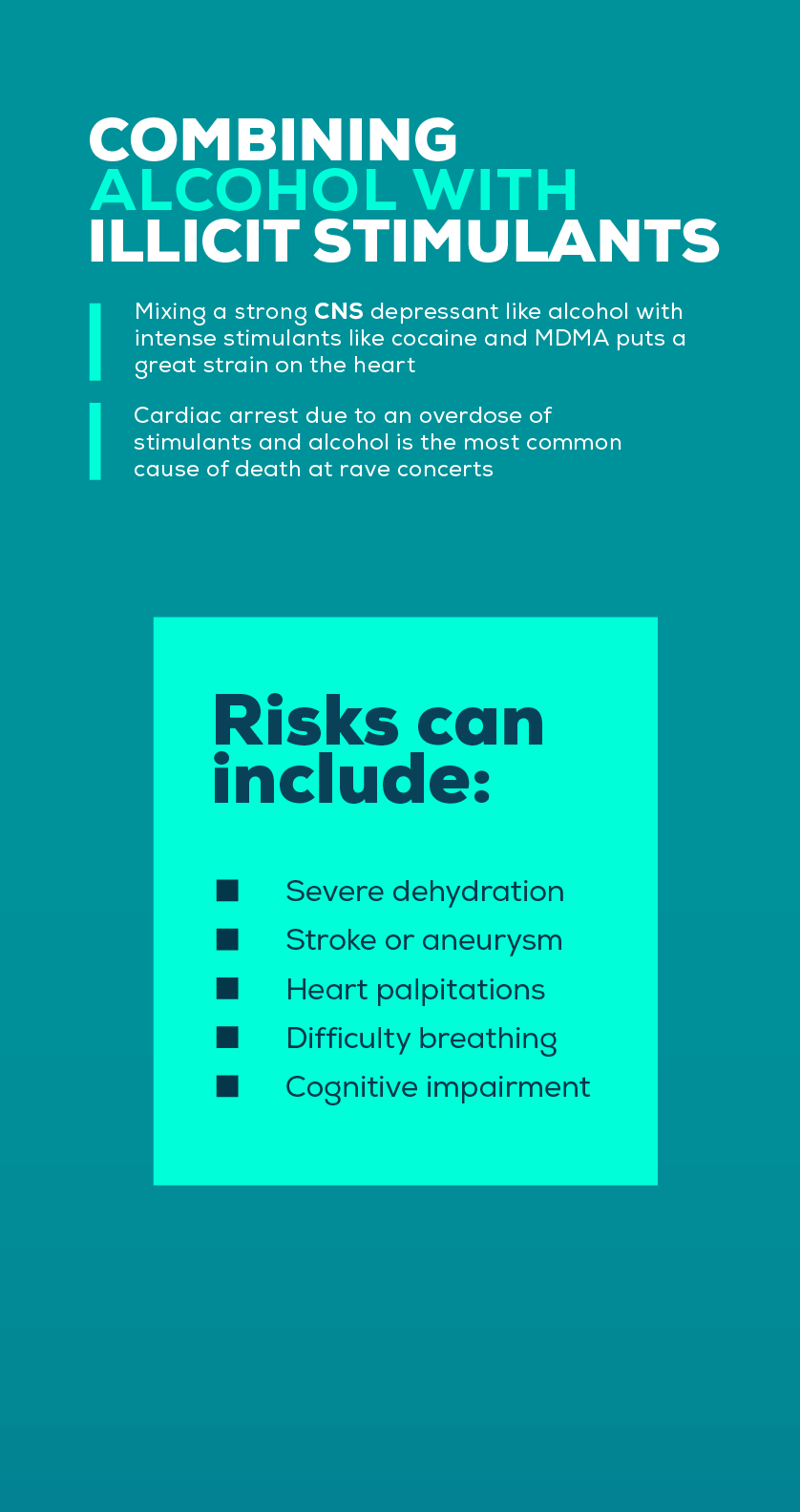
The most common illicit stimulants are cocaine and ecstasy, also called MDMA or Molly. Both of these drugs are used frequently in nightlife party culture, especially at clubs and raves. Of course, in any party scene, alcohol also flows freely, and so it happens on a regular basis that partygoers casually mix illicit stimulants with alcohol. These situations result in thousands of ER visits every year.
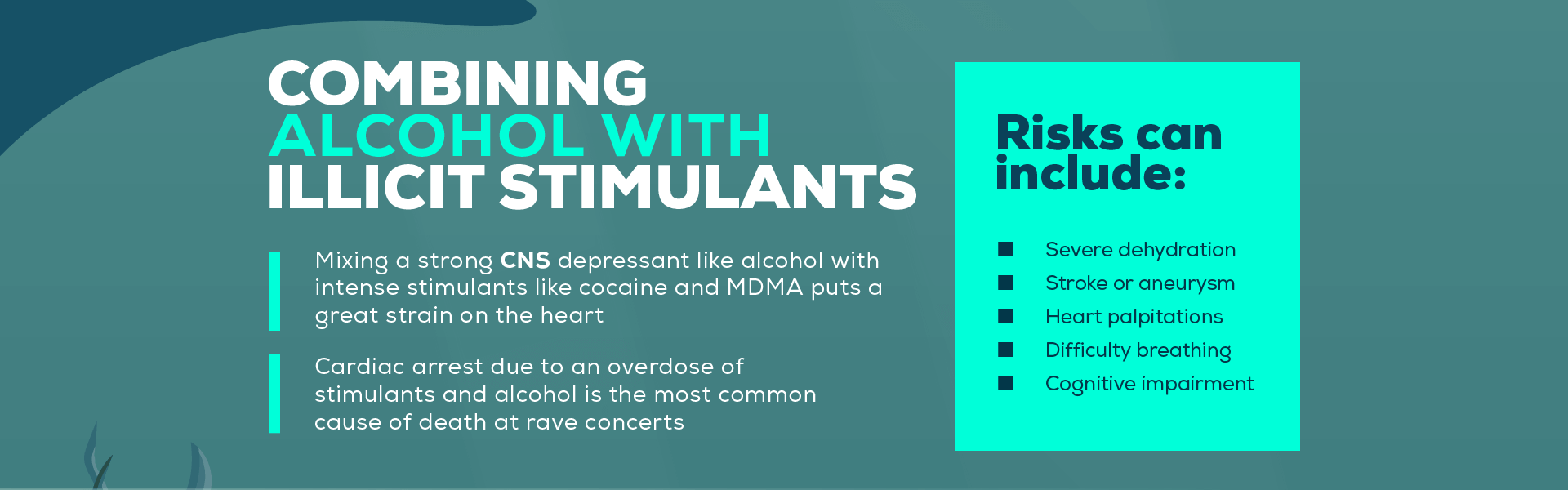

First of all, mixing a strong CNS depressant (alcohol) with intense stimulants like cocaine and MDMA puts a great strain on the heart. Cardiac arrest due to an overdose of stimulants and alcohol is the most common cause of death at rave concerts.
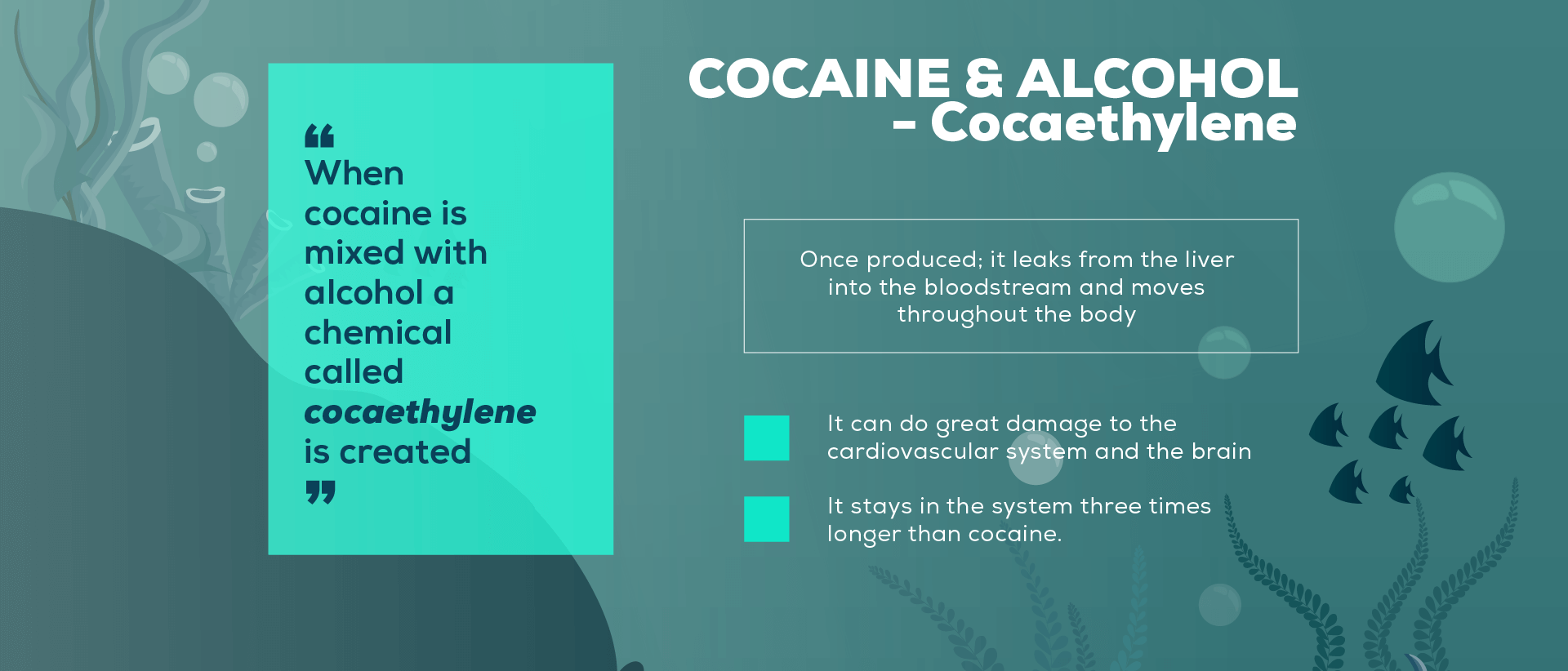
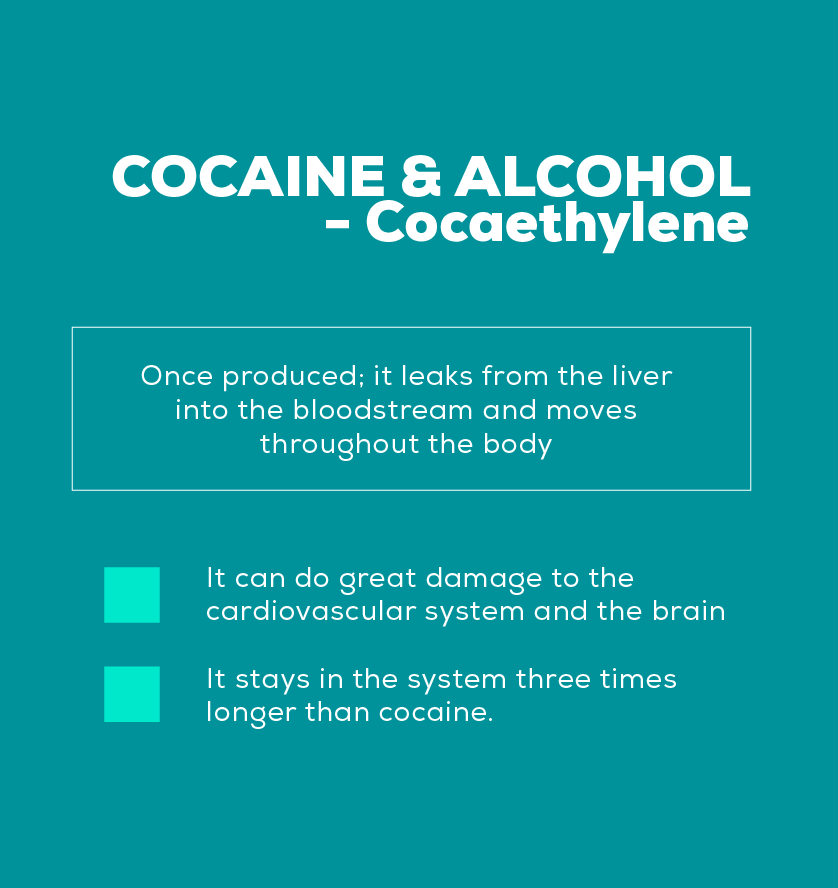
Cocaine in particular presents additional risks when it is mixed with alcohol, since this combination creates a rare chemical called cocaethylene in the liver. Cocaethylene is a byproduct of metabolizing cocaine and alcohol together; once produced; it leaks from the liver into the bloodstream and moves throughout the body. This toxic chemical can do great damage to the cardiovascular system and affects brain health as well. It stays in the system three times longer than cocaine.
Other risks presented by mixing stimulants with alcohol include:
- Severe dehydration
- Damage to the liver and kidneys
- Coma
- Stroke or aneurysm
- Increased blood pressure and heart rate
- Heart palpitations
- Difficulty breathing
- Cognitive impairment
- Loss of motor control and coordination
19. Mixing Meth and Alcohol
Technically, methamphetamine is a stimulant like cocaine and MDMA, but since its side effects are very different from those substances, meth deserves its own section. For one thing, meth users mix drugs with alcohol for different reasons. Alcohol is often consumed after a meth binge to help the user "come down" and fall asleep after days of tweaking.
Despite the seemingly positive effect this might have for a meth addict who hasn't slept in days, it is extremely dangerous behavior. Meth can mask the effects of alcohol, leading to an individual drinking much more than they normally would because they don't feel drunk. This can lead easily to alcohol poisoning. Other dangers of mixing meth with alcohol are:
- An increase of violent and erratic behavior
- Extremely poor decision-making patterns
- Dangerous and unsafe sexual behaviors
- An elevated risk of suicide
- Seizures
- Increased blood pressure and heart rate
- Strain on the heart and possibly cardiac arrest
20. Combining Alcohol with Hallucinogens
Very little research has been done on mixing hallucinogens with alcohol, but the little that exists indicates that combining these two substances is a very bad idea. Hallucinogens include several different types of drugs, all of which can produce hallucinations, visions, and disassociation:
- LSD
- DMT
- Psilocybin
- Peyote
- PCP
- Ketamine
- DXM
- Salvia
Although the side effects of mixing hallucinogens with alcohol vary widely from person to person, there are a few similarities:
- Increased heart rate
- Anxiety and agitation
- Delusions or a "bad trip"
- Extremely erratic and dangerous behavior
- Vomiting and nausea
Overall, the sheer unpredictability and volatile nature of mixing these two substances is reason enough not to consume them. When it comes to hallucinogens, you never know what could happen.
What Should I Do in the Case of a Polydrug Overdose?
If you or someone you know has a history of abusing multiple substances, this individual is at high risk from overdose. It is absolutely vital that you know how to recognize the signs of a dangerous drug interaction or overdose, as well as what to do if it happens.
Although the signs of overdose will vary according the combination of substances taken, all of these are major danger signs that require medical attention:
- Profoundly depressed breathing rate or respiratory arrest
- Severely compromised motor coordination
- Loss of consciousness
- Bluish skin, lips, or fingernails
- Extreme stomach pain
- Irregular heartbeat
- Seizures
- Heart attack
- Dilated pupils
- Unsteady walking
- Chest pain
- Gurgling sounds that indicate the person's airway is blocked
- Abnormally high body temperature
- Excessively violent or aggressive behavior
- Disorientation or confusion
- Extreme paranoia and agitation
- Convulsions or tremors
If you notice any combination of these symptoms, take immediate action. Call 911 or, if you are sober and it is possible, go straight to an emergency room. If you have to wait for medical personnel to arrive, try some of the following measures to keep the situation under control:
- Keep the individual conscious if possible; engage them and keep them talking.
- Check their breathing and heart rate periodically to make sure they do not stop breathing.
- If a person stops breathing, turn them on their side and/or perform CPR if you have the necessary training.
- Follow the instructions of 911 operators over the phone.
- Dispose of all medications, alcohol, and illicit substances that may be available to the overdose victim.
- Obtain information about which substances were taken and when. If any prescription bottles are available, provide those to medical personnel.
- Stay as calm as possible but do not attempt to reason with the overdose victim. Let them know that help is on the way.
Intervention for Polysubstance Use Disorders
If you suspect that someone you care about is suffering from a polydrug addiction, time is of the essence. Polysubstance abuse is extremely dangerous and the sooner the user can get help, the better their chances are at achieving recovery.
Sometimes, addiction to multiple substances creates an even stronger addiction than a single substance could, and the user may be incredibly resistant to the idea of getting drug treatment. You'll lose nothing by trying to help, but if you plan to stage an intervention, make sure you have preparations in place:
- Consult a quality drug rehabilitation center and find an experienced interventionist to help you formulate an effective plan.
- Assemble a team. Besides the interventionist, gather the closest friends and family of the addict who may have the most influence over him or her.
- Do your homework; educate yourself and your intervention team about the nature of addiction, how it works, and how it can be treated.
- Set boundaries and consequences. Each person in the intervention team will formulate specific consequences for the individual if they refuse to get help. These consequences could be things like the cessation of financial support or taking away visitation rights of children, etc.
- Write everything down beforehand in order to clearly get your points across.
- Perform the intervention at a scheduled place and time without prior knowledge on the part of the addict.
- Be prepared to move forward with the stated consequences if the addict refuses help.
Polydrug Addiction and Co-Occurring Disorders
Polydrug addiction can occur when any multiple substances (whether illicit or prescribed by a doctor), including alcohol, are mixed and abused on a regular basis. Researchers have noticed that co-occurring mental health disorders are more common for patients that abuse multiple substances, but it is difficult to say if the mental illness came first, or if chronic drug use brought on the mental illness.
For example, in the case of users who take prescription stimulants for ADHD and later develop an alcohol abuse problem, the attention-deficit disorder clearly came first.
Users who abuse ecstasy and alcohol simultaneously, however, may actually be causing their own mental depression by exhaustively depleting serotonin and dopamine levels in the brain.
Whether the chicken came before the egg or not does not matter as much as getting both the addiction and the mental illness treated. Quality drug rehabilitation centers offer dual-diagnosis treatment, providing full medical diagnoses for various addictions as well as any mental conditions underlying those addictions. Once a dual-diagnosis has been made, doctors and counselors can create a personalized treatment plan to address both the addiction and all mental and emotional disorders that accompany it.
"In order to change the world, you have to get your head together first."
-Jimi Hendrix
Detox for Polydrug Addiction
The withdrawal process from any addiction is painful and extremely difficult. Detoxing from multiple substances at the same time is doubly as excruciating. Since each substance comes with its own unique set of withdrawal symptoms, withdrawing from multiple substances means that you'll be suffering through the combined symptoms of each different drug you've been abusing. For example, cocaine withdrawal creates a variety of severe psychological symptoms while alcohol withdrawal symptoms are often more physically painful. Someone who is addicted to both will have to manage the combined strength of both the psychological and physical withdrawal symptoms.
Another important aspect of polydrug withdrawal is that the process can be more dangerous. Some polysubstance addictions can cause significant damage to the brain, liver, heart, and kidneys, which may limit the treatment options available to relieve withdrawal symptoms. This makes it all the more important to attend a full-service treatment center where the medical personnel have the experience and knowledge necessary to help you through detox without causing any additional damage or dangerous side effects to your body.
In the case of polydrug abuse, full medical and psychiatric examinations will be necessary to determine the state of health in your brain and body before beginning detox. From there, a professional drug treatment team can formulate a personalized detox treatment plan to bring you through polydrug withdrawal safely and as comfortably as possible.
Medical Detox
In certain situations, medically assisted detox can be extremely helpful during polydrug withdrawal. With the right combination of medications, some of the worst withdrawal symptoms can be minimized, making the experience more bearable overall. This is especially important during polysubstance withdrawal since the symptoms are usually more numerous and severe. Some medications may also prevent dangerous withdrawal conditions like delirium tremens in the case of alcohol, or suicidal thoughts in the case of meth or cocaine.
For those who suffer from polydrug addictions, however, medical detox can be more complicated than for single drug addictions. The effects of multiple drug abuse on the brain, heart, liver, or kidneys may prevent the possibility of taking certain detox medications. For this reason, it is of the utmost importance to obtain a personalized medical detox treatment plan from a qualified doctor.

The Final Step: Drug Rehab
No addiction - be it to drugs, alcohol, or some combination of both - can be magically cured by a successful detox. Addiction is a chronic brain disease and polysubstance addiction can have even more powerful control over the brain than a single drug addiction. Once a detox program has been successfully completed, your long-term success will depend on your dedication to the drug rehabilitation treatment you receive afterwards.
You see, detox only addresses the physical side of substance use disorder, but polydrug addictions have much deeper psychological and social roots beyond the physical dependence. A comprehensive drug treatment center will be necessary to help you understand the nature of your own personal addiction, where it stems from, and how to manage it on a daily basis. A good rehab program will teach all of these things as well as practical tools to help you battle the day-to-day triggers and challenges of addiction in the future. This step is inexorable in the journey towards long-term sobriety.
Don't compromise yourself. You are all you've got.
- Janis Joplin
If music legends Janis Joplin or Jimi Hendrix could speak today, would they tell us that one night's bad decision was worth losing all of the promise their young careers held? We doubt it. No matter how dark the path ahead may seem, there are ways to climb out of the gloom that is addiction. Whether it's your own alarming drug abuse habits or someone you love, the time to treat polysubstance abuse is now. This type of addiction is tremendously life-threatening, and each day that passes could be one day too late.

Talk to a Rehab Specialist
Our admissions coordinators are here to help you get started with treatment the right way. They'll verify your health insurance, help set up travel arrangements, and make sure your transition into treatment is smooth and hassle-free.
Contact Us
Share This on Social Media
Source: https://www.northpointrecovery.com/mixing-alcohol-and-drugs/
0 Response to "Does Lithium Make You Blackout From Alcohol Easy"
Post a Comment